Guide to Plantar Fasciitis Treatment
Plantar fasciitis is an inflammation and/or degeneration of a thick band of tissue that runs along the arch of your feet from your heel to your toes and aids in stabilization of your arch while you walk and run.

It is usually under the mid central area of the heel (Green Circle)sometimes on the inner border of the heel and sometimes on the outer border of the heel often radiating into the arch of the foot (Yellow Circle). Occasionally it radiates up into the toes. Usually it affects 1 foot only but sometimes seen in both if not treated.
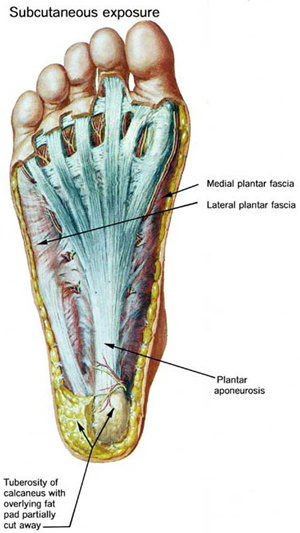
Anatomy
The plantar fascia is a thickened fibrous aponeurosis that originates from the medial tubercle of the calcaneus, runs forward to insert into the deep, short transverse ligaments of the metatarsal heads, dividing into 5 digital bands at the metatarsophalangeal joints and continuing forward to form the fibrous flexor sheathes on the plantar aspect of the toes. Small plantar nerves are invested in and around the plantar fascia, acting to register and mediate pain. The plantar fascia is made up of 3 distinct parts: the medial, central, and lateral bands.
The central plantar fascia is the thickest and strongest section, and this segment is also the most likely to be involved with plantar fasciitis.
In normal circumstances, the plantar fascia acts like a windlass mechanism to provide tension and support through the arch. It functions as a tension bridge in the foot, providing both static support and dynamic shock absorption.
Pathophysiology
Biomechanical dysfunction of the foot is the most common cause of plantar fasciitis; however, infectious, neoplastic, arthritic, neurologic, traumatic, and other systemic conditions can prove causative.
The pathology is traditionally believed to be secondary to the development of microtrauma (microtears), with resulting damage at the calcaneal-fascial interface secondary to repetitive stressing of the arch with weight bearing.
Excessive stretching of the plantar fascia can result in microtrauma of this structure either along its course or where it inserts onto the medial calcaneal tuberosity. This microtrauma, if repetitive, can result in chronic degeneration of the plantar fascia fibers. The loading of the degenerative and healing tissue at the plantar fascia may cause significant plantar pain, particularly with the first few steps after sleep or other periods of inactivity.
The term fasciitis may, in fact, be something of a misnomer, because the disease is actually a degenerative process that occurs with or without inflammatory changes, which may include fibroblastic proliferation. This has been proven from biopsies of fascia from people undergoing surgery for plantar fascia release.
Studies have introduced the etiologic concept of fasciosis as the inciting pathology. Fasciosis, like tendinosis, is defined as a chronic degenerative condition that is characterized histologically by fibroblastic hypertrophy, absence of inflammatory cells, disorganized collagen, and chaotic vascular hyperplasia with zones of avascularity.
These changes suggest a noninflammatory condition and dysfunctional vasculature, which may be seen on ultrasound. With reduced vascularity and a compromise in nutritional blood flow through the impaired fascia, it becomes difficult for cells to synthesize the extracellular matrix necessary for repairing and remodeling.
Correct Diagnosis for Your Heel Pain
Plantar fasciitis is by no means the only cause of heel pain. Listed below are just a few of the many causes of heel pain. Getting the correct diagnosis is key to resolving symptoms.
Diagnosis
Plantar fasciitis is diagnosed based on your medical history and physical examination. During the exam, we check for areas of tenderness in your foot. The location of your pain can help determine its cause.
Imaging tests
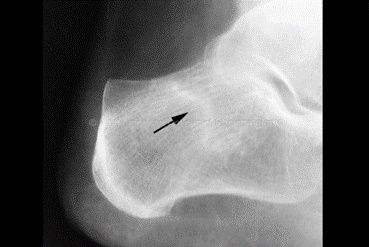
Often no tests are necessary. We might suggest an X-ray Ultrasound scan or magnetic resonance imaging (MRI) to make sure another problem, such as a stress fracture, is not causing you pain.
Sometimes an X-ray shows a piece of bone sticking out (spur) from the heel bone. In the past, these bone spurs were often blamed for heel pain and removed surgically. But many people who have bone spurs on their heels have no heel pain.
Sometimes we also order blood tests to exclude inflammatory diseases.
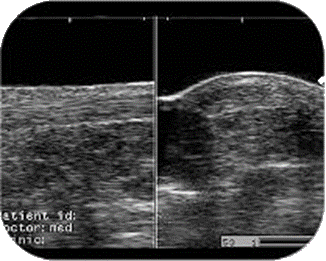
Ultrasound
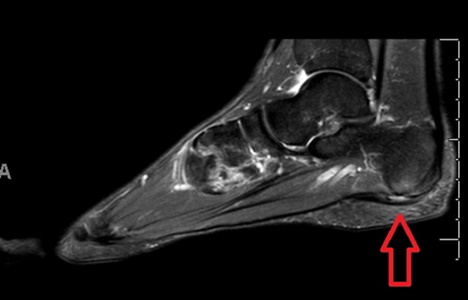
MRI Scan
Differential Diagnoses
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome is an entrapment of the nerve that travels on the inside of the ankle. This condition can cause heel pain that feels very much like plantar fasciitis.
Calcaneal Stress Fracture
A calcaneal stress fracture is a tiny fracture of the heel bone. It often occurs on the bottom of the heel or the back of the heel. If on the bottom of the heel it is often mistaken for plantar fasciitis and if on the back of the heel is often mistaken for Achilles tendonitis.
Baxter’s Nerve Entrapment
Baxter’s nerve (also called the first branch of the lateral plantar nerve) runs direction under the bottom of the heel. If this nerve gets irritated or entrapped it can mimic plantar fasciitis. Thus it is one of the primary diagnoses that is often mistaken for plantar fasciitis.
Calcaneal Bursitis
A bursa is a small fluid filled sac that occurs throughout our bodies in areas of increased pressure. A bursa under the heel can be mistaken for plantar fasciitis. Often we can visualize bursas on ultrasound examination.
Calcaneal Cyst
A bone cyst is a weak or thin area of bone. This can lead to both dull and sharp heel pain. Bone cysts can be be diagnosed with x-ray, CT scans or MRI scans.
Radiculopathy
A radiculopathy is a nerve entrapment in the back. In some patients this can result in pain that presents under the bottom of the heel.
Rheumatoid Arthritis, Psoriatic Arthritis and Other Systemic Arthridities
There are a number of diseases that can present with heel pain. Often patients spend years being treated for plantar fasciitis when the problem is actually a systemic condition. Besides those listed above these can include conditions such as ulcerative colitis, reactive arthritis and Sjogren’s syndrome.
Plantar Fascial Tear
A tear or rupture of the plantar fascia can occur near the heel bone. While the area of the is the same as plantar fasciitis the pain itself is usually more substantial and it can even be difficult to bear weight. Sometimes bruising can be seen after the injury occurs.
Gout
While many people think gout primarily affects the big toe joint it can, in fact, cause pain at the heel. Usually causes severe pain with redness and increased temperature in the area.
Soft Tissue Mass
There are a number of different soft tissue masses that can occur under the heel or just in front of it. These include fatty cysts, ganglion cysts, varicose veins and tumors.
Heel Fat Pad Atrophy or Displacement
There are some conditions that result in the loss of the fatty padding underneath the heel. This can be when there is a direct loss of the fatty padding (eg Some Rheumatoid diseases) or sometimes it is displaced because a lack of integrity of the soft tissue that binds the fat family under the heel (Hypermobility syndromes). This can lead to increased pressure on the under surface of the calcaneum (Heel Bpone) with the possibility of developing bone bruising, stress reactions or fractures of the calcaneum.
Treatment Plan for Plantar Fasciitis
When treating plantar fasciitis I follow this protocol:
For tissue to heal you must first stop damaging it so it has a chance to heal.
There are two types of force that affect the plantar fascia:



Home stretching programs are often the first line of treatment and can be very effective. There are many suggestions for home stretching programs involving numerous stretching exercises.
Based on current research and your individual considerations, we may recommend one or more of the following:
-
Stretching Exercise: Direct Stretch of the Plantar Fascia
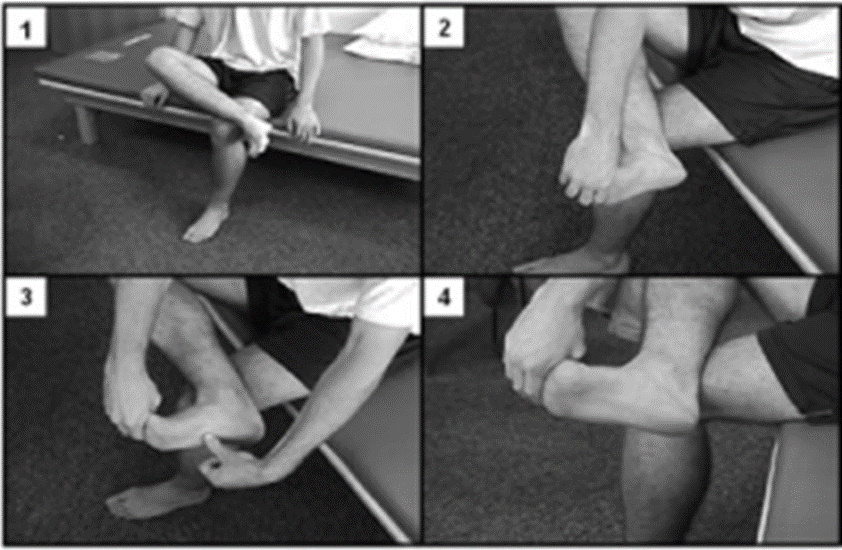
Studies have shown that this stretching technique is the most successful form of stretching for plantar fasciitis. It has been shown to be very effective when combined with orthotics and anti-inflammatory therapies and can help to reduce pain significantly.
This new stretch targets the plantar fascia more effectively than the standard stretch that was long used.
We recommend this stretch be performed before taking the first step in the morning and again after prolonged sitting so that it’s done at least three times per day.
To Perform the direct Plantar Fasciitis Stretch:
-
Continuous stretch: Using a night splint
A number of studies have shown that night splints can be beneficial in helping to treat plantar fasciitis and Achilles tendonitis. Although they have not been shown to be effective if used as the only treatment for heel pain, they seem to work well in conjunction with other therapies.
One 1998 study showed that 80% of patients using night splints saw significant improvement in just one month. And a 2007 study also showed significant improvement with the use of night splints. By maintaining a gentle stretch on your foot while you sleep, a night splint can prevent night time contraction of the tendon and decrease inflammation that causes morning heel pain.

Night splints are one of the best ways to treat morning heel pain. Although night splints are intended to be worn while sleeping, many of our patients find it difficult to sleep while wearing the splint. As an alternative, you can benefit by wearing a night splint during the day for 30 minute intervals while watching TV, reading or working on your computer to speed healing. Plan on using the night splint for the first three to four weeks of treatment.
If both feet hurt, we suggest you initially purchase only one night splint. Even patients that can sleep with one night splint on find it a challenge to sleep wearing two. Those that are back or side sleepers may be more comfortable sleeping while wearing night splints while those that sleep on their stomachs tend to find them less comfortable.
Choosing a night splint – our recommendations
I have reviewed a number of night splints and the following one I find most effective, comfortable and affordable. Click to view
-
High load stretching and strengthening to progressively increase the ability of the plantar fascia to handle greater loads.

Perform one-legged heel raises on a stair with a towel inserted under the toes to elevate the toes or a special tool to help with toe position.
The towel should be thick enough that your toes are bent up as far as they will go at the top of the heel raise. Rather than a towel you can also use the Fasciitis Fighter dev
(The unaffected leg should hang free, bent slightly at the knee.)
To maximize the benefit of this exercise it is important that the toes by bent up to the end of their range of motion.
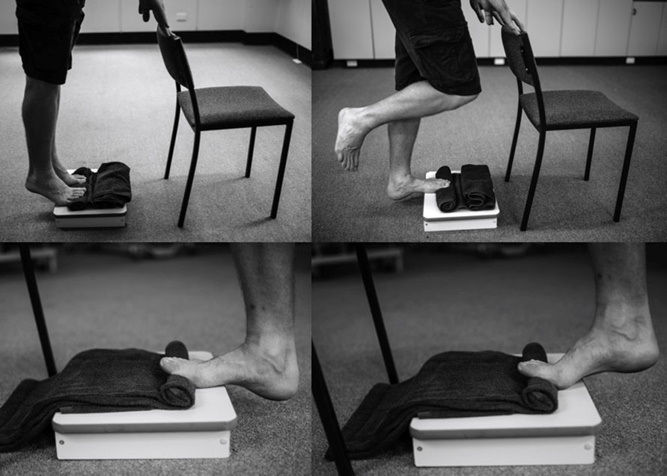
A 2014 study by Ratcliff demonstrated that doing high load strength training has potential to improve plantar fasciitis symptoms faster than just stretching.
Clinical data indicates that this stretching program alone can help in improving the symptoms of Plantar Fasciitis in about 72% of the cases.
Clinical Paper
-
Ice and deep ice massage
Ice is very effective at reducing swelling and pain. Keeping socks on to avoid an ice burn.

1. Place the heel on an ice pack for fifteen minutes three times a day.
2. Deep ice massage. Use a small plastic soft drink bottle.

Injection therapy is used to supplement rehabilitation programs or orthotic therapy when conservative care is failing to make sufficient progress.
We often use diagnostic ultrasound to guide injections to the site that is causing pain. Injections can be given to reduce inflammation (corticosteroid) or to reduce friction and provide nutrient for the joint (hyaluronic acid).

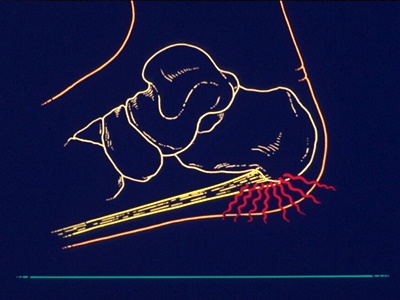
Extracorporal shockwave therapy is a non-invasive, non-surgical treatment option for treatment of ligament and tendon injuries.
“Extracorporeal” means “outside the body”. “Pulse Activation” is a type of shockwave, also known as pressure or sound waves.
These shockwaves are generated from the unit and are focused onto the painful heel tissue. The shockwaves trigger the body’s repair mechanisms.
The concept behind shockwave therapy is that the shockwave stimulates and reactivates healing to encourage new blood vessel formation and other elements necessary to advance normal tissue healing.
Additionally, shockwaves help to over-stimulate pain transmission nerves, which can lead to a reduction in sensitivity and pain.

Keep in mind that this isn’t like a steroid injection where rapid results can be seen. What shockwave does is stimulate the bodies healing process, so it takes a number of weeks to see results.
Most of the best studies show about 70% of patients with chronic heel pain due to plantar fasciitis will find relief with ECSW therapy.
How is the Shockwave Treatment Performed?
Coupling gel is applied to your foot in the area requiring treatment. ECSWT pressure waves are then released via the applicator while moving it over the treatment area.
Is it Safe?
Yes. There are a tremendous number of clinical studies and tests that have confirmed its effectiveness and safety. In fact, for most patients ECSWT has virtually no side effects, risks or complications.

Very rarely if the pain has been present for a very long period and causing distress then surgery may be undertaken to relieve the tension off the plantar fascia and heel bone.